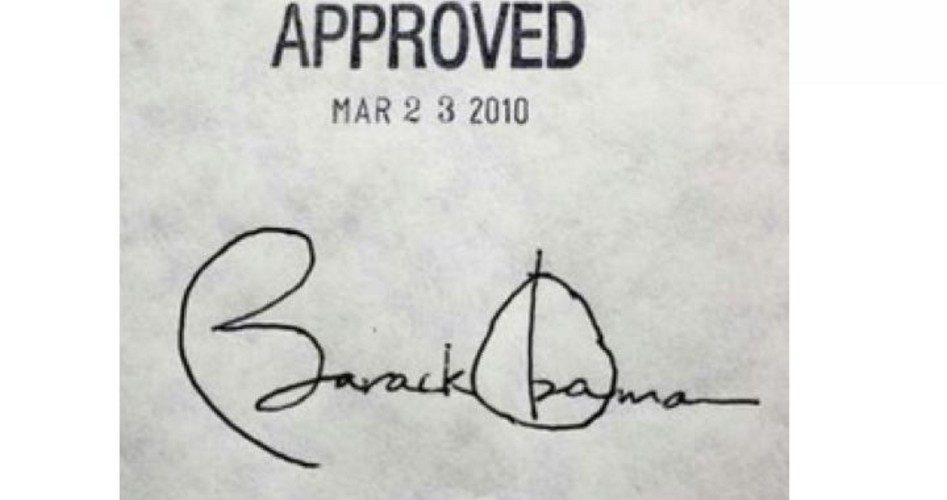
ObamaCare prices will continue to skyrocket for families in 2018, thanks to increasing premium costs and ObamaCare taxes. Premium increases could double and even triple for families at the same time that two new health taxes are set to take effect in 2018, underscoring once more the need to repeal the anything-but-Affordable Care Act.
Consumers who purchase their own coverage and earn too much to qualify for financial aid will bear the biggest burden of price increases. “People have every right to be angry,” said Sabrina Corlette, a researcher and professor at Georgetown University’s Health Policy Institute.
According to Corlette, health insurers had already dramatically raised rates in 2017 to offset the rising healthcare costs. With health insurance companies leaving the marketplace in droves, the remaining ObamaCare insurers are forced to raise prices once again.
The Wall Street Journal reports that major health insurers will be seeking increases as high as 30 percent for premiums on 2018 Affordable Care Act plans. “Big insurers in Idaho, West Virginia, South Carolina, Iowa and Wyoming are seeking to raise premiums by averages close to 30% or more,” according to preliminary rate requests published Tuesday by the U.S. Department of Health and Human Services.
And as high as that 30-percent figure is, it refers to statewide averages. For individuals, the increases can be significantly higher. In Florida, for example, statewide increases will average 45 percent, with some seeing hikes as high as 81 percent. In Charlottesville, Virginia, individual premiums will go up anywhere from 195 percent to 247 percent, the Daily Progress reports.
Doug Gray, executive director of the Virginia Association of Health Plans, told the Daily Progress that the middle class will suffer the most from the premium increases.
“For the people without a subsidy, it’s ridiculous. It’s completely unaffordable. It works very well for people who are at 100 [percent] to 400 percent of the poverty line. It doesn’t work at all if you’re over that.”
Many ACA insurers are claiming that the price increases are a result of the uncertainty surrounding the future of ObamaCare. But this is dishonest as health insurance costs have continually increased since the passage of ObamaCare long before there was a Trump administration to threaten the healthcare law’s future.
The departure of many insurers from the healthcare exchanges is a significant contributing factor to the anticipated price increases, but insurers had little choice after losing millions of dollars on the exchanges. Humana, UnitedHealth Group, Blue Cross, and Anthem, once supporters of the healthcare law, all reported struggles with plans that were sold on the exchanges, indicating that they were not ready for the increased number of particularly high-risk customers, many of whom have generated far more claims than insurers predicted, though critics of the law have from the beginning forecast such outcomes. Consumers in some states have now been left with just one health insurance option.
Meanwhile, on January 1, the Health Insurance Tax (appropriately abbreviated HIT) will deliver another dose of pain to families already struggling to pay for health insurance. The Daily Caller reports:
The HIT, a provision hidden in the Affordable Care Act of 2010, imposes a fee on each health insurance policy companies sell, fees that are then passed on to the consumer. The “excise” tax is not tax deductible, which raises its effective rate by 54 percent. That means, between the actual excise (about $14 billion) and the premium hike needed to cover non-deductibility, the HIT would make health care $22 billion more expensive next year — not $22 billion better, just a lot more money from American businesses and consumers for the same coverage.
A one-year moratorium was placed on the tax in 2017 but is set to expire on December 31 unless Congress acts, increasing payments for 157 million Americans. Over the next 10 years, individuals will see a spike of $2,400; families will be struck with a $7,000 increase.
HIT places small businesses in a particularly bad position, as they will be paying over $500 more per family coverage policy in 2018. According to the National Federation of Independent Business, HIT could cost approximately 286,000 jobs and result in $33 billion in lost sales by 2023.
Congress has introduced legislation to suspend the tax for another two years.
The Cadillac tax on high-cost employer health plans is also supposed to take effect in 2018. The Cadillac tax is a 40-percent excise tax outlined in a section of the Affordable Care Act that targets overly generous employer-provided healthcare plans, placing pressure on employers to offer less-generous health plans.
Republicans have introduced a bill that would implement a one-year delay on the tax and give employers “three years of retroactive relief and one year of prospective relief” from the ACA mandate that they provide insurance to their employees.
But all of these bills are short-term solutions to a very long-term problem. Until ObamaCare is repealed, each New Year will carry with it fears of unaffordable and poor quality health insurance.




