A Texas doctor was arrested Tuesday for allegedly “selling his signature” to process nearly $375 million in fraudulent Medicare and Medicaid claims in a scheme that was carried on for half a decade; $350 million was improperly billed for Medicare and $24 million for Medicaid. In what is being characterized as one of the largest healthcare scams organized by a single doctor, critics are suggesting that the development only solidifies the fact that the government’s Medicare and Medicaid fraud detection system is gravely flawed.
Federal authorities contend that Jacques Roy of the southwestern Dallas suburb of DeSoto, and six other people, certified 11,000 Medicare recipients through over 500 health providers across a five-year period. But an investigation into Roy’s Medicare practice was not initiated until about a year ago.
The alleged scheme operated from January 2006 to November 2011, though specific dollar amounts as to how the funds were distributed among Roy and his six alleged accomplices are not yet available. “Dr. Roy’s company is alleged to have certified more Medicare beneficiaries for home health services, and had more beneficiaries under its care, than any other medical practice in the United States,” U.S. Deputy Attorney General James Cole disclosed during a news conference in Dallas.
The agency that oversees Medicare has two groups of contractors, one that pays claims and another that audits those claims for fraud. But U.S. Health and Human Services (HHS) officials say it is often difficult to track the performance of those contractors assigned to detect Medicare fraud — which is projected to reach $60 billion annually.
Federal officials say the HHS has revamped its data analysis and is diverting from the severely flawed “pay and chase” method. “Indeed until fairly recently it has been extremely difficult to get that kind of real time data… Information technology has not come online as quickly as we would like to see,” conceded HHS Inspector General Daniel Levinson. He added, “We’re now able to use those data analytic tools in ways — in 2012 and 2011 — that no, we really could not have done in years past.”
Roy, along with his six co-conspirators, is facing up to 100 years in prison if he’s found guilty on several counts of healthcare fraud. Roy’s attorney, Patrick McLain, affirmed that he will review the evidence, but he is maintaining that his client is innocent. Moreover, McLain insisted that Roy was not aware of what the other defendants were doing. “Dr. Roy was not at all involved with the business of his practice, and was not a businessman,” McLain stated. “The prior business manager was a tyrant, not a business manager, and probably a thief.”
Officials have accused Roy of approving home health services and collecting a hefty sum of the erroneous billings. CNSNews.com reported:
Some of those indicted alongside Roy are accused of fraudulently signing up patients or offering them cash, free groceries or food stamps to give their names and a number used to bill Medicare. Medicare patients qualify for home health care if they are confined to their homes and need care there, according to the indictment. U.S. Attorney Sarah Saldana said some people supposedly eligible for home care were found working on their cars outside.
Home health services are generally administered when patients are confined to their homes and a physician decides they need such care. Roy purportedly used several home health agencies to secure patients so his company, Medistat, could bill for unnecessary home visits and for services that were never rendered. The doctor was using the agencies as “his soldiers on the ground to go door to door to recruit Medicare beneficiaries,” said U.S. Attorney Sarah Saldana. “He was selling his signature.”
Roy would “make home visits to that beneficiary, provide unnecessary medical services and order unnecessary durable medical equipment for that beneficiary,” the indictment stated. “Medistat would then bill Medicare for those visits and services.”
Roy’s six co-conspirators, who have also been indicted, include his office manager, Teri Sivils, and the owners of five home health agencies associated with the scheme. The Centers for Medicare and Medicaid Services indicated that it will suspend an additional 78 home health agencies that are partnered with Roy’s practice. These agencies have been hauling in a sizable $2.3 million a month.
Mr. Levinson said Roy’s billing is “off the charts,” yet the seemingly obvious error was missed for years by Palmetto GBA, the contractor involved in paying the home health agencies using Roy’s signature, and Health Integrity LLC, the agency appointed to monitor fraud.
“You can’t have 11,000 bills from a single doctor if you’re the number one home health provider in the nation,” contended Patrick Burns, spokesman for watchdog group Taxpayers Against Fraud. “You can’t see that many patients. It’s not physically possible.”
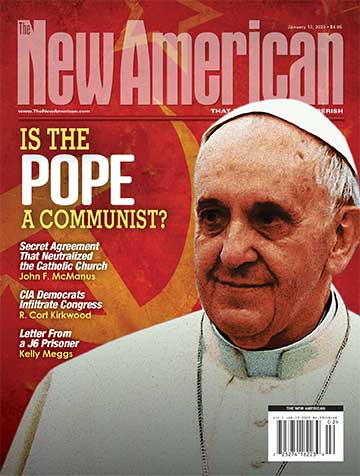
Photo: Dr. Roy’s Medistat office at 2617 Bolton Boone Dr., Desoto, Texas