With brave new “apps” on the market every few weeks, high-tech hearing aids that use radio signals instead of microphones, DNA diagnostics for horrible diseases, and titanium replacements for knees and teeth — all made feasible within the last decade or so — people take for granted breakthroughs in technology and medicine. So, headlines like “Early Signs of Schizophrenia in Child’s Brain Identified”, headlined in various forums last week, didn’t raise many eyebrows.
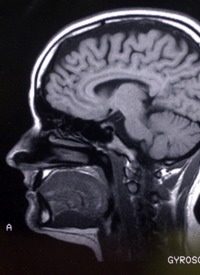
The study, which claims to have detected early schizophrenia, was conducted on the infants of 26 mothers already said to have the affliction (details to be released in September’s American Journal of Psychiatry). The lead expert on the study, John H. Gilmore, professor of psychiatry at the University of North Carolina at Chapel Hill and director of UNC’s Schizophrenia Research Center, claims to have found an anomaly in the male babies’ MRIs — larger brains and larger lateral ventricles (fluid-filled spaces in the brain). Babies of mothers with no psychiatric illness did not have the enlarged ventricles.
Dr. Gilmore speculates that the enlargements might be “an early marker of a brain that’s going to be different” but notes, too, that “larger brain size in infants is also associated with autism,” which is characterized by similar language disturbances. The researchers saw no difference in brain size of female babies in the study, a finding that apparently did not surprise them inasmuch as schizophrenia is more often diagnosed in boys than girls, and “with higher levels of severity.”
In a final caveat, however, researchers cautioned that their findings do “not necessarily mean that boys with larger brains will develop schizophrenia. Relatives of people with schizophrenia sometimes have subtle brain abnormalities but exhibit few or no symptoms.” But “having a first-degree relative with the disease raises a person’s risk of schizophrenia to one in 10.”
Who would not welcome a method of identifying, or screening for, an affliction so that it can be treated fast and early? Especially the kind of malady that screams: “By the time you know you have it, the damage is already done!” Think multiple sclerosis, muscular dystrophy, or diabetes. But this one of many instances where the situation is not as straightforward as it seems.
One big problem leaps off the page in this study: Any mother already diagnosed with schizophrenia will be taking medication — the psychiatric kind. Psychiatric drugs are fraught with side-effects, so much so that patients are advised to obtain a “risk–benefit” analysis if they are planning to become pregnant. In drugs targeting Attention Deficit Disorder (ADD), for example, brain-tissue changes were discovered in patients after the fact. So, mothers ingesting a psychiatric drug, either during or prior to pregnancy, likely will compromise such a study.
Several medical doctors have also pointed out that correlation is not the same as causation. “Cause” for any disease generally implies a culprit common to most, or all, sufferers. The fact that the larger-brain phenomenon applied only to male babies suggests skimpy evidence on which to base a cause-effect relationship.
Considerable controversy surrounds schizophrenia. Classic definitions include (1) abnormalities in perception or expression of reality, as evidenced by “auditory hallucinations, paranoid or bizarre delusions, or disorganized speech and thinking with significant social or occupational dysfunction”; and (2) pressured speech (i.e., speaking incessantly and way too quickly), sudden speech derailment and/or flight of ideas (frequently switching topics in mid-sentence), and thought blocking (obvious interruptions in the train of thought). But schizophrenia also mimics “any of several psychotic disorders characterized by distortions of reality and disturbances of thought and language,” often manifesting as “withdrawal from social contact.” Other ailments featuring similar characteristics are Alzheimer’s disease (a confirmable, physical illness) and even ingestion of alcohol and drugs (legal and otherwise).
Most of the available literature describes schizophrenia as a chronic illness with early onset, but rarely diagnosed before teen years when the “schizophrenic break” occurs — i.e., when the person acts on his or her auditory hallucinations. According to Dr. William K. Summers, a neuroscientist and physician in private practice in Albuquerque, schizophrenics make up the vast majority of the homeless population. “There is waxing and waning of symptoms, but [schizophrenics] never get normal. Medications are a mixed blessing. If your [goal] is to eliminate the ‘voices’, you will create dysfunctional zombies who are medicine non-compliant (these are nasty medications). If your [goal] is functionality, you [work to get] the patient … some control over the ‘voices’ [through psychotherapy].”
Anyone familiar with the story of schizophrenic prodigy John Forbes Nash, Jr., a Nobel Laureate in economics (2001 film adaptation of the 1998 book, A Beautiful Mind), also knows that another all-too-common “therapy” over the years has been electroshock, which frequently destroys the brain and renders the patient not only mentally, but physically, dysfunctional. Lobotomies, chemical and surgical, have been applied to schizophrenics as well. The rationale for extreme measures is that by the time the affliction crosses the stage of preliminary treatment, schizophrenia is difficult or impossible to treat.
But schizophrenia gets, uh, complicated. Retired pediatric neurologist Fred A. Baughman, author of the book The ADHD Fraud — How Psychiatry Makes “Patients” of Normal Children, explains that in medicine, there are organic diseases (physical) and then there are psychological disorders. Dr. Baughman writes: “None of the psychiatric, psychological diagnoses have a pathology or abnormality that anybody so far has been able to determine. In medical terminology, that means gross, microscopic or chemical ‘markers’.”
So that leaves what? A collection of symptoms or patient complaints, in other words, purely subjective phenomena.
Then there are internists like Dr. Jane Orient, executive director of the American Association of Physicians and Surgeons and managing editor of its flagship publication. She basically agrees with Baughman concerning the difficulties inherent in psychiatric diagnoses, as well as the drawbacks of nonconsensual mental health screening and the dangers of mind-altering drugs for children. But she draws the line at painting all mental afflictions with a broad brush, especially schizophrenia and Post-Traumatic-Stress disorder (PTSD). In an interview, she explained:
Schizophrenia is very different from the “trendy” illnesses — a definite component of disordered, bizarre thought, not just exaggerated emotion. It is not a “new” phenomenon like ADD-ADHD (attention-deficit-hyperactivity disorder), generalized anxiety disorder, etc. Drug treatment has been beneficial to many schizophrenics — which is not to say that [psychiatric] drugs can’t be very harmful, especially to people who don’t have schizophrenia. We must remember the history of Soviet psychiatry, which diagnosed dissidents as having … schizophrenia.
One of the most thorough analyses of schizophrenia and other mental illnesses from the psychiatric community emanates from Dr. Michael J. Hurd, a licensed psychotherapist based in Delaware and frequent debunker of “pop” psychology. A major theme espoused by Dr. Hurd is that psychiatry, as a field, should return to psychology. In an article, “Thinking Out of the Box About Schizophrenia,” he writes:
Existing research … acknowledges that no particular gene or combination of genes has been linked to schizophrenia. … There must be more to the whole issue of schizophrenia than the current … research … considers. Modern psychiatry will remain incapable of resolving this problem until it gets itself “out of the box” it has created for itself: taking for granted that thought disorders are entirely genetic, physiological issues.
Given the reality of what we know about schizophrenia …, why do most people still have the impression (generated through the popular media and government) that schizophrenia is primarily, if not exclusively, a biological, genetic disorder waiting for the right pill to come along to wipe it out? No such conclusion is warranted.
Could it be that the conclusions drawn from UNC’s schizophrenia study is an attempt to “medicalize” a psychological affliction by holding up the MRIs of male babies as visible evidence? Might not that advance the cause of biological thought disorders and the concurrent psychopharmaceutical approach to “curing” them?
The trouble is the short step from legitimizing thought disorders to “medicalizing” opinions because, after all, attitudes, opinions and worldviews all stem from thoughts. The benefit-to-risk question then becomes: Who decides whether an opinion or worldview is rational? And, more importantly: Is it ethical to try to “cure” someone’s “irrational” opinion?
_______________
Beverly K. Eakman is a former educator and retired federal employee who served as speechwriter for the heads of three government agencies as well as editor-in-chief of NASA’s newspaper (Johnson Space Center). Today, she is a Washington, D.C.-based freelance writer and columnist, the author of five books, and a frequent keynote speaker on the lecture circuit. Her most recent book is Walking Targets: How Our Psychologized Classrooms Are Producing a Nation of Sitting Ducks (Midnight Whistler Publishers).
Photo: AP Images



